Iron Deficiency Anemia, Iron Deficiency
- See also
- Epidemiology
- Most common cause of Microcytic Anemia (50% of cases)
- Most common micronutrient nutritional disorder worldwide
-
Incidence (U.S.)
- Children 1-5 years: 2-5%
- Rare before age 6 months in term infants
- Rare until birth weight doubles in Preterm Infants
- Associated with delayed cognitive development and higher risk of infectious disease
- Men: 2-3%
- Women (pregnant in third trimester): 25%
- Associated with increased perinatal mortality and Preterm Labor
- Women (non-pregnant): 12% when menstruating
- Children 1-5 years: 2-5%
- References
- Causes
- Children
- Premenopausal women
- Menorrhagia: 2 mg/day iron lost
- Dietary Iron absorption: 1.5 - 1.8 mg/day iron gained
- Each Pregnancy: 500 to 1000 mg iron lost
- Males and Postmenopausal women
- Colon Cancer until proven otherwise
- Gastrointestinal blood Loss
- Gastritis from NSAID use
- Peptic Ulcer Disease
- Partial gastrectomy
- Bariatric Surgery (Gastric Bypass)
- Diverticulosis
- Gastrointestinal Angiodysplasia
- Ulcerative Colitis
- Celiac Sprue
- Increased iron requirements
- Pregnancy (see above)
- Childhood
- Uncommon Causes
- Gastrointestinal Parasites (e.g. Hookworms)
- Gastrointestinal blood loss in long distance Running
- Hereditary Hemorrhagic Telangiectasia
- Pulmonary Hemosiderosis
- Risk Factors
- Menorrhagia
- Low socioeconomic status
- Chronic Kidney Disease
- Decreased iron absorption
- Proton Pump Inhibitor use
- Bariatric Surgery history (esp. Roux-en-Y Bypass)
- Increased iron utilization
- History
- Nutritional history
- Infants
- Exclusively Breastfed infants (Iron Supplementation starting at age 4 months)
- Infant formula should contain iron
- Children
- Excessive cow's milk intake
- Teens and adults
- Infants
- Blood loss history
- Change in stool color (Melena or bright red blood)
- History of excessive menstrual flow (Menorrhagia)
- Recent surgery
- Recent pregnancy or delivery
- Frequent blood donation or lab blood draw
- Bleeding Disorders
- Hemodialysis
- Hemolytic Anemia
- Gastrointestinal condition history or Family History
- Medications
- Agents affecting iron absorption
- Chronic Antacid use (esp. Proton Pump Inhibitors)
- Agents predisposing to GI Bleeding
- Agents affecting iron absorption
- Symptoms
- See Pica
- Iron Deficiency may be symptomatic even without Anemia
- Symptoms of Iron Deficiency Anemia
- Pica
- Dizziness
- Dyspnea or Fatigue on exertion
- Restless Leg Syndrome
- Tinnitus
- Palpitations
- Irritability (infants)
- Attention Deficit Hyperactivity Disorder (children)
- Signs
- See Anemia Signs
- Alopecia
- Atrophic Glossitis
- Brittle Nails
- Angular Cheilitis
- Dry Skin
- Koilonychia
- Pallor (including mucosal pallor)
- Tachycardia
- Associated Conditions
- Generalized Pruritus
- Restless Leg Syndrome
- Glossitis
- Angular Cheilitis
- Fatigue
- Developmental Delay in children
- Labs
- First-Line Studies
- Complete Blood Count with Hemoglobin, MCV and RDW
- Serum Ferritin
- Serum Iron, Total Iron Binding Capacity and Transferrin Saturation (optional if Serum Ferritin is low)
-
Complete Blood Count (CBC)
- See Hematocrit Cutoffs for Anemia
- Hemoglobin
- See Hemoglobin Cutoffs for Anemia
- Anemia values (WHO)
- Men: Hemoglobin <13 g/dl (130 g/L)
- Non-pregnant women: Hemoglobin <12 g/dl (120 g/L)
- Pregnancy and children age <5 years: Hemoglobin <11 g/dl (110 g/L)
- Mean Corpuscular Volume (MCV)
- General
- See MCV Cutoffs for Microcytic Anemia
- MCV cutoff varies by age and per reference
- MCV usually <75 in Iron Deficiency Anemia
- MCV >95 fl virtually excludes Iron Deficiency (Test Sensitivity >97%)
- Normocytic Anemia (MCV 80 to 100 fl)
- Normocytic early in course of Anemia
- Normocytic erythrocytes are found in 40% of Iron Deficiency patients
- Microcytic Anemia (MCV <80 fl)
- Microcytosis follows Hemoglobin drop of 2 g/dl
- General
- Red Cell Distribution Width (RDW)
- Precedes change in Mean Corpuscular Volume
- Mean Corpuscular Volume to Red Blood Cell Count ratio
- See Mentzer Index
- Ratio <13: Thalassemia
- Ratio >13: Iron Deficiency Anemia, Hemoglobinopathy
-
Iron Studies (in order of sensitivity)
- Serum Ferritin <30-45 ng/ml (usually <15-20 ng/ml)
- Falls before other indices
- Most sensitive for Iron Deficiency Anemia
- Serum Ferritin <30ng/ml is 92% sensitive and 98% specific for Iron Deficiency in age >5 years
- Serum Ferritin <12 ng/ml suggests Iron Deficiency in age <5 years
- Falsely elevated as acute phase reactant
- Serum Ferritin <50 ng/ml cutoff is used in Iron Deficiency with inflammatory states
- Serum Ferritin >100 ng/ml excludes Iron Deficiency despite inflammatory state
- Total Iron Binding Capacity (TIBC) rises
- Serum Iron
- Falls after Serum Ferritin
- Falls after Total Iron Binding Capacity (TIBC)
- Transferrin Saturation decreased (<5-9%, with some guidelines using <20%)
- Serum Iron to Total Iron Binding Capacity
- Falls after Serum Ferritin
- Serum Transferrin receptor assay (new)
- Increased in Iron Deficiency Anemia
- Normal in Anemia of Chronic Disease
- Serum Ferritin <30-45 ng/ml (usually <15-20 ng/ml)
- Other diagnostic tests (indicated in unclear diagnosis)
- Soluble Transferrin Receptor
- Indirect measure of Erythropoiesis
- Increased in Iron Deficiency
- Not affected by inflammatory states
- Erythrocyte Protoporphyrin level
- Heme precursor
- Increased in Iron Deficiency
- Similar timing as with Transferrin Saturation
- Bone Marrow Biopsy
- Indicated when diagnosis is unclear despite above testing
- Soluble Transferrin Receptor
-
Reticulocyte Count or Reticulocyte Index
- Does not assess degree of Iron Deficiency Anemia
- Useful in categorization of Anemia type (distinguish from non-Iron Deficiency causes)
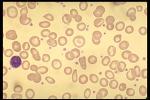
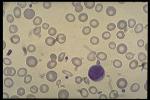
- Images
- Differential Diagnosis
- Management
- General
- Review general Anemia management in specific cohorts
- Identify a source of blood loss
- Manage known blood loss sources (e.g. Menorrhagia)
- High correlation to Colon Cancer in older patients (up to 9%)
- Exercise caution in adult men and postmenopausal women with Iron Deficiency Anemia
- Bidirectional endoscopy (EGD, Colonoscopy) is recommended
- Ioannou (2002) Am J Med 113:276-80 [PubMed]
- Consider non-malignant occult gastrointestinal losses
- Peptic Ulcer Disease (and consider Helicobacter Pylori testing)
- Inflammatory Bowel Disease
- Celiac Sprue
- Management
- Iron Supplementation
- Daily Iron absorption and utilization is limited
- Bone Marrow response limited to 20 mg/day elemental iron
- Hepcidin is secreted by the liver in response to oral iron intake
- Hepcidin suppresses iron absorption for the next 24-48 hours after Iron Ingestion
- Hepcidin triggers ferroportin degradation in enterocytes and Macrophages
- Hepcidin is also increased in chronic disease (e.g. CHF, CKD, infection)
- Iron intake more than once daily is unlikely to significantly raise body iron stores
- Iron taken every other day may be just as effective as once daily iron intake
- Typical adult dosing
- See Ferrous Sulfate for administration precautions
- Iron absorption reduced up to 40% when taken with meals (also reduced with Calcium, tea, coffee)
- Further absorption is reduced with gastric acid hyposecretion (e.g. Proton Pump Inhibitor use)
- Ferrous Sulfate
- Standard dose: 325 mg orally daily (65 mg elemental iron daily)
- Twice daily dosing (130 mg elemental iron) was often recommended initially
- Continue Ferrous Sulfate 325 mg orally daily for at least 3 months
- Additional 1-3 months may be required to replenish iron stores
- Lower dose: 15-20 mg elemental iron
- Low dose (15-20 mg) is as effective as 65-130 mg/day with less adverse effects
- Lo (2023) Eur J Haematol 110(2):123-30 +PMID: 36336470 [PubMed]
- Standard dose: 325 mg orally daily (65 mg elemental iron daily)
- See Ferrous Sulfate for administration precautions
- Anticipated response
- Hemoglobin increases 1 gram/dl every 2-3 weeks
- Iron stores normalize after Hemoglobin is corrected
- May require additional 4 months to normalize
- Example timeline
- Week 1: Reticulocytosis begins by day 4 of oral iron
- Week 2: Reticulocytosis (<10%)
- Week 3: Increased Hemoglobin increases 1-2 g/dl (10-20 g/L)
- Week 4: Recheck Hemoglobin And if <1 g/dl increase, consider IV iron
- Week 8: Recheck Hemoglobin And iron studies and consider extending Iron Supplementation for 1-2 months
- Evaluate failure to respond to Iron Supplementation
- Noncompliance
- Poor iron absorption due to concurrent medications
- Continued excessive blood loss
- Consider Parenteral Iron if true malabsorption
- Consider iron refractory conditions
- Malabsorption
- Vitamin B12 Deficiency
- Zinc Deficiency
- Chronic Kidney Disease
- Hematopoietic disorders
- Hepcidin dysregulation
- Resources
- Patient Education
- Information from your Family Doctor: Iron Deficiency