Chronic Lymphocytic Leukemia, CLL
- See Also
- Epidemiology
- Most common Leukemia in the United States
- Older patients
- Usually over age 50 years
- Age over 65 years old in 70 to 85% of new cases
- More common in men
- Rare in Asian patients
- Pathophysiology
- Neoplastic accumulation of mature Lymphocytes
- Involves Blood and Bone Marrow
- May infiltrate Spleen and Lymph Nodes
- Clonal B Lymphocyte mass involved in 95% of cases
- Chromosomal Abnormality: Trisomy 12
- Symptoms
- Asymptomatic in 50 to 70% of patients
- Leukocytosis often found incidentally on Complete Blood Count (CBC)
- Constitutional and generalized symptoms
- Other presentations
- Frequent infections
- Labs
-
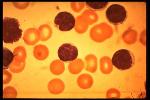
Peripheral Smear
- Leukocytosis
- Morphologically normal small Leukocytes
-
Complete Blood Count
-
Leukocyte count 15,000 to 200,000 (80-90% mature)
- Clonal expansion of >5000 B Lymphocytes/mm3
- Decreased Platelet Count
- Hemoglobin or Hematocrit consistent with Anemia
-
Leukocyte count 15,000 to 200,000 (80-90% mature)
-
Electrocardiogram (EKG)
- Obtain baseline EKG prior to treatment and as needed
- Diagnosis
-
Leukocytosis or Hyperleukocytosis is present in both CLL and CML
- White Blood Cell Count is >20,000/mm3 in most cases, and often >100,000/mm3 (Hyperleukocytosis)
- Contrast with normal white cell counts or Leukopenia associated with Acute Leukemias
- CLL is often asymptomatic at time of diagnosis
- Chronic Lymphocytic Leukemia (CLL) specific findings
- Significant increase of normal appearing Lymphocytes (>50% of cells)
- Peripheral blood for clonal expansion of B Lymphocytes >5000/mm3, and confirmed by flow cytometry
- Bone Marrow Biopsy is not needed for diagnosis (but defines extent of marrow involvement related to prognosis)
- Differential Diagnosis
- B-Cell CLL
- Reactive Lymphocytosis
-
T-Cell CLL
- Sezary Syndrome
- Adult T-Cell Leukemia
-
General
- Prolymphocytic Leukemia
- Lymphosarcoma Cell Leukemia
- Hairy Cell Leukemia
- Waldenstrom's Macroglobulinemia
- Complications
- Pancytopenia
- Coombs-positive Hemolytic Anemia (20%)
- Hypogammaglobulinemia
- Opportunistic infection
- Richter's Syndrome (evolves into aggressive Lymphoma)
- Autoimmune Thrombocytopenia
- Imaging
-
Chest XRay
- Enlarged mediastinal Lymph Nodes
- Management
- Treatment
- Indications for active management
- Active stage disease
- Worsening constitutional symptoms
- Worsening Lymphocytosis, Thrombocytopenia, Anemia
- Worsening Lymphadenopathy, Hepatosplenomegaly
- Efficacy of treatment
- No regimen effective at eradicating CLL
- Goal is to reduce Leukemia cell mass and symptoms
-
Alkylating Agents (pulsed q3-6 weeks or continuous)
- Indications
- Hemolytic Anemia and other cytopenia
- Disfiguring Lymphadenopathy
- Symptomatic organomegaly
- Marked systemic symptoms
- Agents
- Indications
-
Glucocorticoids
- Coombs-positive Hemolytic Anemia
- Immune Thrombocytopenia
- Pancytopenia
- "Packed Marrow" Syndrome
- Splenectomy indications
- Hypersplenism
- Refractory Hemolytic Anemia
- Thrombocytopenia
-
Radiation Therapy indications
- Localized disease
- Palliative end-stage disease therapy (total-body)
- Other agents
- Small molecule inhibitors (e.g. Venetoclax)
- Immunoglobulin transfusion (not proven efficacious)
- Management
- Surveillance for those under observation only (no treatment)
- Indications for observation only (no active treatment)
- Anemia absent AND
- Thrombocytopenia absent AND
- Fewer than 3 Lymph Node regions involved
- Repeat history and physical exam every 6 to 12 months (evaluate for progression to active disease)
- Periodic constitutional symptom history every 6 to 12 months
- Fatigue
- Weight loss
- Night Sweats
- Fever
- Periodic exam every 6 to 12 months
- Hepatosplenomegaly
- Complete skin exam
- Periodic Labs every 6 to 12 months
- Complete Blood Count (CBC with differential)
- Hematology Consultation for Anemia or Thrombocytopenia
- Periodic constitutional symptom history every 6 to 12 months
-
Vaccination
- Influenza Vaccine yearly
- Pneumococcal Vaccine every 5 years
- Covid19 Vaccine
- Avoid Live Vaccines in patients being monitored without treatment
- Routine cancer screening (appropriate for age and gender)
- Management
- Surveillance for those who have been treated
- Cardiology Consultation for baseline examination
- Periodic Echocardiogram (rest and stress)
- Frequency depends on risks and Echocardiogram findings
- Course
- Indolent nature
- Often incidental finding on Complete Blood Count
- Staging
- Stage A: Lymphocytosis (<3 Lymph Node groups involved)
- Median survival: over 10 years
- Stage B: Lymphocytosis (>3 Lymph Node groups involved)
- Median survival: 5 years
- Stage C: Lymphocytosis with Anemia or Thrombocytopenia
- Median survival: 2 years
- Prognosis
- Age <50 years old: 93% five-year survival
- Age 50 to 64 years old: 91% five-year survival
- Age >65 years: 80% five-year survival