Hip Fracture, Femur Fracture, Femoral Fracture
- Epidemiology
- Osteoporosis Related
- Age of onset
- Most are over age 65 years
- Mean age of Hip Fracture 80 years old
- U.S. Incidence of Hip Fracture at age 65
- Overall: 300,000 per year
- Men: 4-5 per 1,000 (lifetime Prevalence 10%)
- Women: 8-10 per 1,000 (lifetime Prevalence 20%)
- Worldwide gender distribution of Hip Fracture
- Men: 30%
- Women: 70%
- Morbidity and Mortality
- Mortality 20-30% within 1 year Hip Fracture
- Men: 31% mortality in 1 year
- Women: 17% mortality in 1 year
- ADL assistance needed in 50% of Hip Fractures
- Long term care needed in 16 to 25% of Hip Fractures
- Bedridden longterm in 11% of Hip Fractures
- Walking Aid needed in 80% of Hip Fractures
- Mortality 20-30% within 1 year Hip Fracture
- References
- Risk Factors
- Non-modifiable
- See Osteoporosis Risk Factors
- Age over 65 years
- Women over age 85 years have a 10 fold increased risk over women age 60 to 70 years
- Female gender
- Family History of Hip Fracture
- Past history of Hip Fracture or any Fracture
- Female gender
- Lower socioeconomic status
- Fall Risk
- Deconditioning and decreased mobility
- Metabolic bone disease
- Malignancy involving bone (pathologic Fracture)
- Risk Factors
- Modifiable
- Low Body Mass Index (BMI) <18.5 kg/m2
-
Osteoporosis with Low Bone Mineral Density (BMD T-Score < -2.5)
- Present in 50% of Hip Fractures
- Physical inactivity (minimal weight bearing)
- Doubles Hip Fracture risk
- Low Vitamin D levels
- Medications lowering Bone Mineral Density
- Medications increasing Fall Risk
- Lifestyle
- Moderate to high Alcohol use (>1 oz Alcohol or >27 grams Alcohol per day)
- Tobacco Abuse
- Excessive Caffeine intake (>3 cups of coffee daily)
- Precautions
- Low mechanism Trauma may result in Hip Fracture, with comorbid Osteoporosis or malignancy
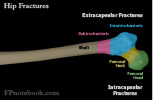
- Types
- Hip Fracture
- Images
- Hip Fractures account for 87% of Femur Fractures
- Intracapsular Fracture: Femoral Neck Fracture (45 to 53% of all Hip Fractures)
- Non-displaced Femoral Neck Fractures are the most commonly initially missed Fractures (9-10%)
- Higher risk of AVN, nonunion, malunion or degeneration
- Minimal cancellous bone, thin periosteum, poor blood supply
- Types
- Subcapital Femur Fracture (proximal neck Fracture)
- Transcervical neck Fracture (mid-neck Fracture)
- Extracapsular Fracture
- Intertrochanteric Fracture (38 to 50% of all Hip Fractures)
- Good blood supply and largely cancellous bone
- Heals well with ORIF
- Subtrochanteric Fracture (3% of all Hip Fractures)
- Often requires intramedullary rods or nails
- Higher risk of impact failure
- Femoral Shaft Fracture (or lower Femur Fracture, 5% of all Hip Fractures)
- Intertrochanteric Fracture (38 to 50% of all Hip Fractures)
- Trochanteric Fracture (Hip Avulsion Fractures in young, active patients)
- Stress Fractures (frequently missed cause of anterior hip or Groin Pain)
- Symptoms
- Signs
- Shortened limb on Fracture side
- Deformity present in most cases (except in non-displaced Fracture)
- Hip externally rotated and abducted
- Tenderness to palpation over injured hip
- Ecchymosis is a late finding
- Limited and painful range of motion (especially hip rotation)
- Do not test ROM unless XRay normal
- Resisted passive range of motion
- Unable to perform active Straight Leg Raise
- Pain with Log Roll maneuver (gentle internal and external rotation of lower leg and thigh)
- Exam
- Careful and repeated neurovascular exam (In addition to evaluation of Fracture specific signs as above)
- Perform leg Neurologic Exam (sensory, motor, Deep Tendon Reflexes)
- Perform vascular exam
- Imaging
-
Hip XRay
-
Cross Table lateral and anteroposterior views
- Usually identifies Fracture
- Do not perform frog leg view
- Risk of displacement of a non-displaced Fracture
-
Hip XRay may miss non-displaced Femoral Fractures
- Consider MRI or CT for negative XRay with higher index of suspicion
- Parker (1992) Arch Emerg Med 9(1): 23-7 [PubMed]
- Hakkarinen (2012) J Emerg Med 43(20: 303-7 +PMID:22459594 [PubMed]
-
Cross Table lateral and anteroposterior views
- CT Hip
- Test Sensitivity: 87%
- May miss Trabecular Bone injury or Fracture line associated marrow edema
- However, may be useful in evaluation for concurrent Pelvic Fracture
-
Ultrasound
- Test Sensitivity: 100% (operator dependent)
- May identify joint effusion, Hematoma or Fracture line
- Hip MRI (T1-weighted)
- Indicated for high suspicion despite normal XRay
- Test Sensitivity: 100%
- Does not require delay after injury
- Hip Bone Scan with Technetium Tc99m Polyphosphate
- Test Sensitivity: 98%
- Delay scan at least 72 hours after time of injury
- Differential Diagnosis
- See Hip Pain
- Management
- Acute, emergent management
- ABC Management
- Bilateral large bore intravenous lines (transfusion may be required)
- Strongly consider regional Nerve Block in hip and Femur Fractures
- PENG Block (preferred)
- Provides Regional Anesthesia to most of the hip and femur
- Does not block the posteromedial hip capsule (innervated by sciatic nerve)
- Fascia Iliaca Block
- Provides Regional Anesthesia of the proximal femur (anteromedial thigh) to the knee
- Femoral Nerve Block
- Provides Regional Anesthesia covering proximal femur to the knee
- Efficacy
- Hip Peripheral Nerve Blocks are safe with a very low Incidence of nerve injury (0.03%) and LAST Reaction (0.01%)
- Blocks improve pain management, decreases Opioid use, Delirium, and other complications (e.g. Pneumonia)
- Femoral Nerve Block and Fascia Iliaca Block are equally effective at offering excellent Anesthesia
- PENG Block (preferred)
-
Hare Traction Splint in Femur Fracture (typically Femoral Shaft Fracture)

- Traction has not been found to be beneficial in Hip Fracture or Femoral Shaft Fracture
- Does not decrease blood loss or reduce the Fracture
- May decrease pain on transport
- May be helpful in pulseless extremity after Femoral Shaft Fracture
- References
- Orman and Ramadorai in Herbert (2017) EM:Rap 17(6): 9-10
- Handoll (2011) Cochrane Database Syst Rev (12): CD000168 [PubMed]
- Management
- Perioperative management
- See specific Fracture management
- Early surgery within 24-48 hours lowers risk
- Lowers 1 year mortality and Pulmonary Embolism risk (and also lowers Pneumonia and skin breakdown risk)
- Even a delay >24 hours increases mortality at 30 days
- Pincus (2017) JAMA 318(20): 1994-2003 [PubMed]
- Early surgery allows for earlier mobilization, rehabilitation and functional recovery
- Stabilize comorbidities within 72 hours if unstable
- Accelerated surgery time (<6 hours) decreases complications, mobilization time and hospital length of stay
- Lowers 1 year mortality and Pulmonary Embolism risk (and also lowers Pneumonia and skin breakdown risk)
- Thromboembolic Prevention
- See DVT Prevention in Perioperative Period
- Start LMWH or similar agent within 12 hours of surgery (was extended from 4 hours due to bleeding risk)
- Use intermittent pneumatic compression until patient is ambulatory
- Continue prophylaxis for 35 days (instead of prior 10-14 days)
- Aspirin has been shown in some studies to offer equivalent efficacy to Anticoagulants
- Prevention of infection
- See Surgical Antibiotic Prophylaxis
- Protocol: Staphylococcus Aureus prevention
- No Beta-lactam allergy: Cefazolin 1-2 g, one to two hours before surgery and then every 8 hours for 24 hours
- Beta-lactam allergy: Vancomyin 1 g within 1 hour surgery and then every 12 hours for 24 hours
- Remove Foley Catheter within 24 hours of surgery
-
Hemorrhage Management
- Blood Transfusion (pRBC) indicated in hemolobin <8 g/dl
- Prevention of Delirium
- Observe for medical causes
- Electrolyte abnormalities
- Inadequate pain control
- Occult infection
- Avoid medications predisposing to Delirium
- Avoid Polypharmacy
- Avoid Anticholinergics
- Use Regional Anesthesia in place of Opioids (see above)
- Consider treatment if no cause identified
- Low dose Haloperidol, Risperidone, Olanzapine
- Observe for medical causes
- Surgical care is appropriate even at end of life
- Pain control is significantly improved after repair
- Actual intraoperative risk is low
- Complications are typically post-operative
- Nonoperative Indications
- Non-operative care (in place of surgical repair) increases mortality 4 fold at one year
- May consider nonoperative care in non-ambulatory, severely debilitated or end-of-life
- Management
- Rehabilitation
- Early rehabilitation and weight bearing started in first 24 hours after surgery improves mobility outcomes
- Evaluate for Skilled Nursing Facility on day 1 post-op
- Prefracture functionality poor (e.g. ADLs difficult)
- Impaired cognitive function
- Patient can perform therapy 2-3 hours daily
- Protocol
- Day 1: Quadriceps contractions, Gentle Hip ROM
- Day 2-3: Parallel bars
- Day 3-5: Advance to weight bearing with walker/cane
- Assistive Devices
- Complications
- Avascular necrosis
- Increased Risk for Mortality, Long Hospital Stays and Complications
- Age >70 years with Hip Fracture AND
- High Frailty Index
- Fried Frailty Phenotype Criteria
- CSHA Frailty Scale (Rockwood)
- EFrailty (Harvard collection of 5 scales)
- References
- Prevention
- See Osteoporosis Prevention
- See Fall Prevention in the Elderly
-
Physical Activity reduces Hip Fracture risk
- Exercise program to include low to moderate aerobic Exercise, Resistance Training, proprioception training
- Walking 4 hours per week or more (55% reduction)
- Dose dependent effect: 6% reduction per MET-hour/week
- Standing 10 hours per week also reduced risk
- Feskanich (2002) JAMA 288:2300-6 [PubMed]
- Guirguis (2018) JAMA 319(16): 1705-16 [PubMed]
- Tai Chi may reduce risk of fall with injury by 50%
- Exercise program to include low to moderate aerobic Exercise, Resistance Training, proprioception training
- Prevention of recurrent Hip Fracture
- Calcium supplement 1000 mg orally daily
- Vitamin D 800 IU daily supplementation
- Also obtain Vitamin D Levels and initiate full Vitamin D Replacement if <10 ng/ml
- Bisphosphonates
- Additional management if low Bone Mineral Density at time of Hip Fracture (e.g. Parathyroid analogs, RANKL inhibitors)
- References
- Gurr in Marx (2002) Rosen's Emergency Med, p. 655-60
- Huddleston (2001) Mayo Clin Proc 76:295-8 [PubMed]
- Brunner (2003) Am Fam Physician 67(3):537-42 [PubMed]
- LeBlanc (2014) Am Fam Physician 89(12): 945-51 [PubMed]
- Rao (2006) Am Fam Physician 73(12):2195-202 [PubMed]
- Schroeder (2022) Am Fam Physician 106(6): 675-83 [PubMed]