Cerebral Venous Thrombosis, Cerebral Venous Sinus Thrombosis, Thrombosis of Cerebral Vein, Thrombophlebitis of Cerebral Vein, Cerebral Vein Thrombophlebitis, Cerebral Infarction due to Cerebral Venous Thrombosis, Lateral Sinus Thrombosis, Transverse Sinus Thrombosis, Superior Sagittal Sinus Thrombosis, Sagittal Sinus Thrombosis, Sigmoid Sinus Thrombosis, Deep Venous Cerebral Thrombosis, Great Cerebral Vein Thrombosis, Cortical Vein Thrombosis, Superficial Cerebral Vein Thrombosis, Cerebral Sinus Thrombosis, CVST
- See Also
- Epidemiology
- Accounts for 0.5 to 1% of all Cerebrovascular Accidents
- Female gender in two thirds of cases
- Younger patients (mean age 33 years old)
- Pathophysiology
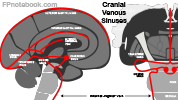
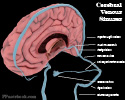
- See Cerebral Sinus
- Images
- As with other Venous Thromboembolism, virchow's triad applies to pathogenesis (stasis, vessel wall, Coagulopathy)
- Venous obstruction causes increased venous pressure and decreased capillary perfusion
- Initial compensation with venous dilation including collateral veins
- Blood brain barrier is disrupted
- Results in vasogenic edema and possible cerebral Hemorrhage
- Cerebrospinal fluid absorption may also be blocked, increasing Intracranial Pressure
- Results in decreased Cerebral Perfusion Pressure, cerebral ischemia and cytotoxic edema
- Hydrocephalus may develop, with increasing Intracranial Pressure and risk of Cerebral Herniation
- Risk Factors
- Precautions
- More than 85% of Cerebral Venous Thrombosis patients have at least one risk factor for thrombosis
- Hormonal
- Oral Contraceptives
- Tamoxifen
- Hormone Replacement Therapy
- Pregnancy or Postpartum State (up to 6 weeks after delivery)
- Most common cause in developed countries
- Accounted for >10% of cases in one study
- Medications
- Asparaginase
- Corticosteroids
- Methotrexate
- Cytotoxic drugs
-
Hypercoagulable Conditions (Thrombophilia, present in 30% of CVT patients)
- See Thrombophilia
- Malignancy (esp. Hematologic Malignancy, myeloproliferative disorder)
- Vasculitis or Inflammation (e.g. Systemic Lupus Erythematosus, Inflammatory Bowel Disease, Behcet's Disease)
- Antiphospholipid Antibody Syndrome
- Hyperhomocysteinaemia (MTHFR gene mutation)
- Factor V Leiden Mutation
- Antithrombin Deficiency
- Protein C Deficiency
- Protein S Deficiency
- G20210A Mutation
- Hematologic Conditions
- Head and Neck Disorders
- Head and Neck Infections (e.g. paramenigeal infections of the ear, sinus or oropharynx)
- Most common cause in developing countries
- Central Nervous System Infections
- Recent neurosurgery
- Closed Head Injury
- Dural AV Fistula or Arteriovenous Malformation
- Head and Neck Infections (e.g. paramenigeal infections of the ear, sinus or oropharynx)
- Miscellaneous Conditions
- Precautions
- Early diagnosis is key to good prognosis
- Frequently missed diagnosis
- Mimics other acute neurologic conditions
- Requires specific testing in most cases (venogram)
- Consider in atypical Cerebrovascular Accident (CVA)
- Young patients
- Pregnancy or recent postpartum
- Infarcts that cross typical arterial distributions
- Multiple infarcts
- Associated atypical features (Altered Mental Status, Seizures, Headache)
- Findings
- General
- Findings are specific to venous sinus involved
-
Headache (90% of cases, and only symptom in 25% of cases)
- New or different Headache
- Acute to insidious onset progressive over hours to days (contrast with Thunderclap Headache in SAH)
- Provoked when Increased Intracranial Pressure (e.g. valsalva, coughing)
-
Increased Intracranial Pressure
- Papilledema
- Visual changes
- Nausea or Vomiting
- Focal Findings
- Encephalopathy (esp. deep sinus involvement)
- Altered Mental Status (esp. in elderly)
-
Intracranial Hemorrhage
- Present in up to 40% of CVT patients (secondary to Increased Intracranial Pressure)
- Bilateral parenchymal hemorrhagic lesions or Hemorrhages across multiple arterial territories
- Findings
- Transverse Sinus Thrombosis
- Accounts for 44 to 73% of cases
- Isolated, noninfectious unilateral thrombosis
- Symptoms may be mild (e.g. Headache) if no infarction
- Seizures
- Contralateral Hemiparesis, hyperreflexia, or spasticity (pyramidal symptoms) may be present
- Left Transverse Sinus (with venous infarction, occluded vein of Labbe)
- Contiguous Sinus extension (e.g. Superior Sagittal Sinus)
- Increased Intracranial Pressure (Intracranial Hypertension)
- Altered Level of Consciousness
- Cranial Nerve Palsy (CN 9-12)
- Cerebral Vein Extension
- Findings
- Superior Sagittal Sinus Thrombosis
- Accounts for 39-62% of cases
-
Increased Intracranial Pressure (Intracranial Hypertension)
- Isolated in many cases
- Focal venous infarction related symptoms
- Headache
- Blurred Vision, Vision Loss or Hemianopsia (Visual Field Deficit)
- Nausea or Vomiting
- Cranial Nerve Palsy
- Aphasia
- Hemiparesis or hemi-sensory loss
- Seizures
- Findings
- Sigmoid Sinus Thrombosis
- Accounts for 40-47% of cases
- Mastoid region pain
- Cranial Nerve Deficit (CBN 6-8)
- Findings
- Deep Venous Cerebral Thrombosis (e.g. Great Cerebral Vein of Galen)
- Accounts for 10-11% of cases
- Altered Mental Status (encephalopathy to coma)
- Motor deficits
- Fluctuating or alternating paresis (or bilateral)
- Findings
- Cortical Vein Thrombosis (Superficial Cerebral Vein Thrombosis)
- Accounts for 3-17% of cases
- Thrombosis involving superficial veins (superficial middle and anastomotic cerebral veins)
- Seizures
- Focal neurologic deficits depending on distribution of thrombosis
- Findings
- Cavernous Sinus Thrombosis
- See Cavernous Sinus Thrombosis
- Accounts for 1-2% of cases
- Headache
- Eye Pain
- Chemosis
- Proptosis
- Cranial Nerve Palsy (CN 3, 4, and 6, as well as opthalmic branch CN 5)
- Fever (if septic Thrombophlebitis)
- Labs
- See Cerebrovascular Accident
- Bedside Serum Glucose
- Complete Blood Count
- Basic Metabolic Panel
- Coagulation studies (INR, aPTT)
- Erythrocyte Sedimentation Rate or C-Reactive Protein
- Serum Troponin
-
Thrombophilia labs
- Obtain before Anticoagulation initiated (consult neurology, hematology)
- Other testing
- Evaluate for other triggering events (systemic or CNS Infection)
- D-Dimer does not exclude Cerebral Venous Sinus Thrombosis
- Diagnostics
- Electrocardiogram
-
Optic Nerve Sheath Diameter
- Increased diameter is a marker of Increased Intracranial Pressure (Papilledema)
-
Lumbar Puncture
- Consider in suspected Meningitis or Encephalitis
- Differential Diagnosis
- Imaging
- Non-Contrast Head CT
- Low Test Sensitivity for Cerebral Venous Thrombosis (~33%)
- Findings consistent with Cerebral Venous Thrombosis
- Delta Sign
- Posterior Superior Sagittal Sinus hyperdensity
- Venous Cerebral Infarction
- Infarct spans more than one arterial perfusion regions
- Diffuse cerebral edema
- Hydrocephalus
- Subarachnoid Hemorrhage (secondary)
- Delta Sign
- CT Venogram (with CT Head)
- Gold standard study for venous cerebral thrombosis
- CTV identifies filling defects
- Similar efficacy to MRV except in Altered Level of Consciousness or encephalopathy (parenchymal lesions)
- Magnetic Resonance Venogram (MRI/MRV)
- As with CT Venogram, gold standard for Cerebral Venous Thrombosis diagnosis
- MRV is preferred over CT venogram for patients with Altered Level of Consciousness or encephalopathy
- Suggests possible deep cerebral vein thrombosis (better visualized on MRV)
- General Findings
- DWI hyperintense
- Cerebral venous wall enhancement
- Thrombosed sinuses with decreased or absent flow
- Findings vary by timing from onset
- Week 1: T1W/T2W isointense to hypointense
- Week 2: T1W/T2W hyperintense
- Management
- Consult Neurosurgery and Stroke Neurology
- Consult hematology in suspected Thrombophilia
- Initiate Low Molecular Heparin (e.g. Lovenox) which is preferred over Unfractionated Heparin
- Use Unfractionated Heparin in Unstable Patients who may require invasive procedure
- Initiate Anticoagulation with Warfarin with INR target 2-3 for 3-12 months
- Limited evidence for DOACs in CVT as of 2020, and therefore Warfarin is preferred
- Dabigatran (Pradaxa) also has some evidence for use
- First episode of CVT: 3-6 months (6-12 months if no known risk factor)
- Continue Anticoagulation lifelong for recurrent CVT
- Endovascular intervention considered in decompensating or refractory cases
- Manage Increased Intracranial Pressure
- See Acute Severe Intracranial Pressure Management
- Acute monitoring by neurosurgery if risk of Increased Intracranial Pressure
- Cerebral Herniation is the most common cause of death in acute Cerebral Venous Thrombosis
- Manage Seizures
- Antiepileptic drugs are indicated for clinical evidence of Seizures and are continued for >=1 year
- Complications
- Persistent Focal Neurologic Deficits
- Hydrocephalus and Increased Intracranial Pressure
- Cerebral Herniation
-
Seizures
- Seen in up to 44% of cases in early Cerebral Venous Thrombosis (up to 30% present with Seizure)
- Seizure does not predict prognosis or mortality
- Kalita (2012) Seizure 21(8): 639-42 +PMID:22840965 [PubMed]
- Prognosis
- Mortality: 4.3% in 2004
- Decreased from 50% in 1967, likely due to early recognition and improved diagnostics
- Recurrent Venous Thrombosis risk off of Anticoagulation
- Recurrent Cerebral Venous Thrombosis (>50% who recurr, do so in first year)
- Within first year: Up to 15% recurrence rate
- After first year: 2-7% recurrence per year
- Recurrent Venous Thromboembolism (e.g. DVT, PE): 4-7% per year
- Recurrent Cerebral Venous Thrombosis (>50% who recurr, do so in first year)
- Poor prognostic factors
- Age >35 years old
- Fever
- Altered Level of Consciousness or Coma
- Increased inracranial pressure or Papilledema
- Focal Neurologic deficits
- Banakar (2017) J Neurosci Rural Pract 8(2):204-8 +PMID:28479793 [PubMed]
- References
- Alfalasi (2022) Crit Dec Emerg Med 36(3): 3-6
- Lively and Clare (2022) Crit Dec Emerg Med 36(5): 4-10
- Marcolini and Swaminathan in Herbert (2021) EM:Rap 21(2): 5-7
- Ulivi (2020) Pract Neurol 20:356-67 [PubMed]