Cardiac Electrophysiology Anatomy, Cardiac Conduction System, Cardiac Action Potential, Heart Conduction Anatomy, Sinoatrial Node, SA Node, Atrioventricular Node, AV Node, Atrioventricular Bundle, AV Bundle, Bundle of His, Kent-His Bundle, Atrioventricular Fasciculus, Purkinje Fiber, Cardiac Cycle, Wiggers Diagram
- Anatomy
- Images
- Cardiac Conduction
 Lewis (1918) Gray's Anatomy 20th ed (in public domain at Yahoo or BartleBy)
Lewis (1918) Gray's Anatomy 20th ed (in public domain at Yahoo or BartleBy)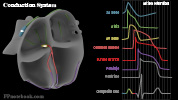

- Cardiac Cycle (Wiggers Diagram)
- Physiology
- Nerve Impulse Transmission
-
Nerve Impulse (Action Potential)
- See Nerve Impulse
- As with Neurons, specialized cardiac Muscle transmits electrical signals
- Vagus Nerve, SA Node and AV Node signals are relatively rapid (similar to Neurons)
- Prominent Voltage-Gated Sodium channel mediated depolarization
- Atrial Muscle, and especially Purkinje Fibers and Ventricular Muscle tend to have sustained impulses
- Prominent Voltage-Gated Calcium channel mediated depolarization
- Sustained impulse results in stronger atrial and ventricular contraction
- Also results in delayed repolarization (refractory period) protecting against rapid Heart Rates
- Sinoatrial Node (SA Node)
- Cluster of cells located at the junction of the superior vena cava and the right atrium
- The SA Node cell spontaneously generate an electrical signal, depolarizing in adults at 60-100/min
- SA Node assumes the Pacemaker function of the heart due to its intrinsic faster rate
- Other cardiac tissue also generate spontaneous signals, but at slower rates
- Electrical signals pass into the right and left atrial Muscles resulting in atrial contraction
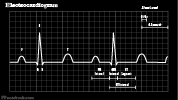
- Atrial Muscle depolarization is detected on Electrocardiogram as P Wave
- Electrocardiogram does not detect the SA Node firing or atrial repolarization
- Signals then continue into the AV Node
- The SA Node is perfused by the right Coronary Artery in 50% (remainder by left circumflex artery)
- Atrioventricular Node (AV Node)
- Small cluster of specialized cardiac Muscle Cells in the interatrial septum near the coronary sinus
- AV Node slows electrical conduction, long enough to allow for ventricular filling after atrial contraction
- The AV Node depolarizes spontaneously at 40-60/min if the SA Node signal is absent
- Gives rise to the Atrioventricular Bundle which passes the electrical signal from the atria to the ventricles
- The AV Node is perfused by the right Coronary Artery in 90% (remainder by left circumflex artery)
- Purkinje Fibers
- Band of specialized cardiac Muscle fibers efficiently and rapidly transmit electrical signals to ventricles
- Atrioventricular Bundle (including the left and right bundles) are composed of Purkinje Fibers
- Atrioventricular Bundle (AV Bundle, Bundle of His, Kent-His Bundle, Atrioventricular Fasciculus)
- Purkinje Fibers transmit electrical signals from the AV Node to the Ventricles
- Electrical signals via the Atrioventricular Bundle resulting in Ventricular Contraction (systole)
- The ventricular Muscle depolarizes spontaneously at 20-40/min if the SA Node and AV Node signals are absent
- Atrioventricular Bundle divides into the left bundle (left ventricle) and right bundle (right ventricle)
- Rapid transmission of signals along the Purkinje Fibers ensures simultaneous ventricular contraction
- Physiology
- Cardiac Action Potential
- See Action Potential
- Images
- Background
- Cardiac Action Potential varies by location within the heart's electrical system
- Classic 4 phase Action Potential reflects ventricular depolarization
- Phase 0
- Phase 1
- Phase 2
- Plateau phase
- Low membrane conductance
- Activation of slow inward Calcium current
- Phase 3
- Outward Potassium current
- Results in repolarization to resting potential
- Phase 4
- Physiology
- Autonomic System Mediators
- See Regulation of Circulation
-
Sympathetic Nervous System (increases Cardiac Output)
- Norepinephrine acts at cardiac cells beta-1 Adrenergic Receptors
- Increases myocardial contractility
- Increases Calcium influx with each Action Potential (resulting in stronger contraction)
- Increases Heart Rate
- Increases SA Node firing and Action Potential conduction velocity (via Sodium, Calcium influx)
- Positive Mediators
- Alpha 1 Adrenergic ReceptorAgonists
- Vasoconstriction and increased cardiac contractility
- Examples: Phenylephrine, Norepinephrine, Epinephrine
- Alpha 2 Adrenergic ReceptorAntagonistS
- Beta 1 Adrenergic ReceptorAgonists
- Increases myocardial contractility (inotrope) and Heart Rate (chronotrope)
- Examples: Norepinephrine, Epinephrine
- Beta 2 Adrenergic ReceptorAgonists
- Vasodilation and bronchodilation
- Examples: Albuterol
- Alpha 1 Adrenergic ReceptorAgonists
- Negative Mediators
- Alpha 1 Adrenergic ReceptorAntagonists
- Alpha Adrenergic Antagonist (e.g. Prazosin, Terazosin, Doxazosin)
- Antihypertensives that reduce Peripheral Vascular Resistance
- Alpha 2 Adrenergic ReceptorAgonistS
- Alpha Adrenergic Central Agonist (e.g. Clonidine, Methyldopa, Aldomet, Guanabenz, Wytensin)
- Antihypertensives that reduce Peripheral Vascular Resistance (also reduce contractility, Heart Rate)
- Beta 1 Adrenergic ReceptorAntagonists
- Selective Beta Blockers (e.g. Metoprolol, Bisoprolol, Atenolol)
- Decrease Heart Rate and cardiac contractility (as well as Cardiac Output)
- Slows AV Node conduction, suppresses SA Node rates, ectopic atrial foci
- Inhibit renin release from renal juxtaglomerular cells (hence lowering Blood Pressure)
- Decreases cardiac workload and therefore cardiac oxygen demand (Antianginal effect)
- Beta 2 Adrenergic ReceptorAntagonists
- Adverse effect of non-selective Beta Blockers (e.g. Propranolol) resulting in bronchospasm, vasospasm
- Peripheral Acting Adrenergic Antagonist
- Block Norepinephrine release from postganglionic nerve terminals
- Examples: Reserpine, Guanethidine, Guanadrel
- Alpha 1 Adrenergic ReceptorAntagonists
-
Parasympathetic Nervous System (decreases Heart Rate)
- Decreases Heart Rate
- Vagal Nerve released Acetylcholine acts at SA Node, AV Node and Atrial Muscle
- Acetylcholine increases SA Node permeability of Potassium
- Membrane resting potential hyperpolarized and less susceptible to depolarization
- Decreases SA Node firing and Heart Rate
- Decreases AV Node Action Potential conduction velocity
- Decreases Atrial Muscle Contractility
- Vagal Nerve released Acetylcholine acts at SA Node, AV Node and Atrial Muscle
- Marginal effect on reducing myocardial contractility
- Sympathetic effect on contractility is dominant
- Decreases Heart Rate
- Physiology
- Other Mediators
-
Sodium-Potassium Pump Inhibitors

- Digoxin (Digitalis) is a Sodium-Potassium ATPase Inhibitor
- Agents that decrease Sodium-Potassium pump (Sodium efflux from cell) increase intracellular Sodium
- Delays AV Node conduction and prolongs AV Node refractory period
- Blunts Atrial Tachycardias
- Extracellular Calcium may exchange with intracellular Sodium to increase intracellular Calcium
- Increased intracellular Calcium increases myocardial contraction strength
-
Calcium Channel Blockers
- Decrease Calcium influx into cell
- Dihydropiridine Calcium Channel Blockers (e.g. Nifedipine) primarily target peripheral vessels
- Vasodilates by reducing vascular smooth Muscle Contraction
- Non-Dihydropiridine Calcium Channel Blockers (e.g. Diltiazem) target both cardiac tissues and vessels
- Vasodilation as with Dihydropyridines
- Decreased cardiac contractility
- Slows Heart Rate by delaying SA and AV Node repolarization
- References
- Goldberg (2014) Clinical Physiology, Medmaster, Miami, p. 35-50
- Guyton and Hall (2006) Medical Physiology, Elsevier Saunders, Philadelphia, p. 103-30

