Epiphyseal Fracture, Growth Plate Fracture, Salter Fracture, Salter-Harris Fracture, Physeal Injury
- See Also
- Epidemiology
- Epiphysis involved in 20% of Pediatric Fractures
- Distal radius is the most commonly involved Physeal Injury (44%)
- Pathophysiology
- See Growth Plate (Physis)
- Children have Growth Plates that are much weaker than ligaments (by a factor of 2-5 fold)
- Joint Trauma that would otherwise cause a ligamentous sprain in adults, results in a physeal Fracture in children
- Physeal Fractures may occur with minimal overlying Soft Tissue Injury
- However, suspect a concurrent type 3-4 physeal Fracture, when children sustain a Ligament Sprain
- Grading
- Mnemonic for Salter Fracture (SALTER)
- Same as the epiphysis or Slip or Separate the epiphysis from the shaft
- Above the Physis (proximal to the Physis)
- Low anatomic or lower than the Physis (Below or distal to the Physis)
- Through the Growth Plate (Epiphysis and Metaphysis)
- Everything (Compressed)
- Round, ruined or Rang
- Grading
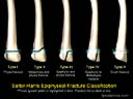
- Salter-Harris classification
- Salter I
- Most common in newborns and young children (9% of Growth Plate injuries overall)
- Fracture line through the Growth Plate (Physis)
- XRay is typically normal (or Physis may be wider) until callus formation is visible by 10 days after Fracture
- Diagnosed clinically based on point tenderness over the epiphysis
- Managed with Splinting and then Casting
- Prognosis excellent
- Salter II
- Most common overall Epiphyseal Fracture (75% of Epiphyseal Fractures)
- Similar to Type 1
- Bony Fracture triangular fragment known as Thurston-Holland Fragment
- Up to 50% displacement will completely remodel and heal within 1.5 years
- Distal Radius Fractures are most common Type II Salter Harris Fracture
- Distal Tibia Type II Fractures are higher risk for premature physeal closure and angular deformity
- Treated with immobilization (Casting or Splinting)
- Prognosis excellent with immobilization (although joint instability is possible)
- Salter III
- Uncommon and more complicated Fracture
- Similar to Type 2, but intraarticular Fracture through epiphysis
- May disrupt the Epiphyseal Plate proliferative and reserve zones
- Risk of Delayed Growth and post-Traumatic Arthritis
- Alignment is critical for good prognosis and maintained function
- Immobilize and obtain urgent orthopedic Consultation
- Consider reduction
- ORIF is often necessary (if instability or >2mm articular surface displacement)
- Salter IV
- Accounts for 12% of Fractures
- Intraarticular Fracture extending completely through Growth Plate and out of metaphysis
- Needs perfect reduction (often open reduction is required)
- Poor prognosis, lost blood supply and high risk of growth failure (especially femur or tibia)
- May result in focal fusion of bone and joint deformity
- Salter V
- Rare Fracture (<1% of Epiphyseal Fractures) requiring severe mechanism (e.g. fall from height)
- Crushing of Physis, most commonly in knee or ankle
- Reserve zone of Physis is disrupted, resulting in loss of vascular supply
- Results in arrest of bone growth, impaired function and extremity length discrepancy
- Early XRay negative (similar to Type I in this regard)
- Subsequent xrays demonstrate callous formation and delayed bone growth
- Diagnose clinically based on point tenderness
- Splint with orthopedic follow-up
- Poor prognosis
- Salter VI (Rang)
- Portion of Growth Plate sheared off
- Penetrating injuries
- Rare
- Exam
- Approach: Every Extremity Injury
- Mnemonic: "joint above, joint below, circulation, motor and Sensation, skin and compartments"
- Include examination of joint above and below the involved joint
- Include Sensory Exam, Motor Exam, Reflex Exam and vascular exam (pulses, Capillary Refill)
- Include skin and compartment exam
- Mallon (2013) Shoulder Disorders, EM Bootcamp, Las Vegas
- Specific to grwoth plate injury
- Joint line and Growth Plate tenderness
- Joint instability (Ligament Sprain)
- Compare with opposite limb
- Bony deformity
- Precautions
- Red Flags suggestive of Physeal Injury
- Point tenderness over a Growth Plate (regardless of xray findings)
- Inability to bear weight
- Ligamentous sprain or instability in a child (commonly associated with underlying Grade 3-4 physeal Fracture)
- Ankle Sprain with rotation and supination is a risk for Tillaux Fracture, esp ages 12-15 (high risk injury)
- Imaging
- Management
-
Analgesics
- Acetaminophen and Ibuprofen
- Opioids may be needed
- Fracture reduction
- Follow-up with orthopedics or sports medicine
- Prompt follow-up within 7-10 days for all suspected Growth Plate injuries
- Urgent follow-up for all suspected Grade 3-5 Salter-Harris Fractures
- Repeat XRay in 7-10 days
- Review risks related to Growth Plate Fractures with patients and their families
- Physeal arrest (5-10% of all Growth Plate Fractures)
- Risk of bone growth arrest and Limb Length Discrepancy or angular deformity
- Indications for non-removable splint (if any doubt, Splinting is safest approach)
- Splint all Salter-Harris Fractures (with positive xray or suspected based on exam findings)
- Splint injuries with significant tenderness over the Growth Plate despite negative XRay
- Lower extremity injuries should be non-weight bearing with use of Crutches
- Indications for removable splint (pre-fabricated) or no splint (with follow-up for repeat exam)
- Minor Trauma AND
- Minimal tenderness AND
- Retained function (e.g. weight bearing)
- References
- Claudius and Newman in Herbert (2015) EM:Rap 15(9): 2-3
- Hocker et al (2016) Crit Dec Emerg Med 30(9):3-8
- Sanghani, Kern and Mehta (2025) Crit Dec Emerg Med 39(2): 27-35
- Peterson (1994) J Pediatr Orthop 14(4): 423-30 [PubMed]
- Salter (1963) J Bone Joint Surg Am 45(3): 587-622 [PubMed]